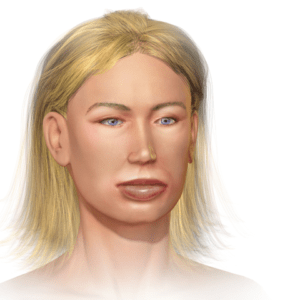
78 years old lady presented to A&E department with h/o lip swelling for past 3 hours. There was no breathing difficulty, itching or skin rash. Her past medical history included AF, hypertension and IHD. She was on Rivaroxaban and Ramipril plus other medications. There was no h/o allergic reaction in the past. She was not commenced on any new medications recently and there was no h/o insect bite.
On examination she had significant swelling of both lips. There was no tongue swelling or stridor. Her vitals were as follows:
Temp. 36.8 C
PR- 90/ min, irregular
B.P. 146/92
O2 saturation: 96% on room air
Heart and lungs examination was normal.
My learning:
What is the pathophysiology of angioedema?
Most common causes of angioedema are mediated by histamine or bradykinin.
Histamine-mediated angioedema, also called allergic angioedema, is a type I IgE-mediated hypersensitivity immune response of mast cell degranulation. This reaction occurs with previous sensitization to allergens such as insect stings, foods, and drugs. [1]
Bradykinin-induced angioedema is the most common cause of non histamine-mediated angioedema.
Bradykinin-mediated angioedema comprises three distinct types:
- hereditary angioedema (HAE)
- acquired angioedema &
- angiotensin-converting enzyme inhibitor (ACEi)-induced angioedema
Angiotensin-converting enzyme is one of the two enzymes that degrade bradykinin; ACEis can cause accumulation of bradykinin that results in angioedema. [2]
ACEI-induced angioedema occurs in 0.1-0.7% of patients treated with these agents.[3]
How to differentiate ACE inhibitor induced angioedema from type 1 hypersensitivity reaction?
Histamine induced angioedema has rapid onset, usually <1 hour after exposure to allergen.
It is commonly associated with itching, urticaria and wheezing.
Patient may also develop hypotension or shock.
It responds quickly to antihistamines, steroids and Adrenaline.
ACE inhibitors induced angioedema is usually slow onset and progress over several hours.
It is confined to face, mostly lips and tongue.
Patients don’t have urticaria, itching or hypotension as seen in histamine induced angioedema.
It does not respond or there is only minimal response to anti histamines, steroids or adrenaline.
How to treat ACE inhibitor induced angioedema?
The first step is to consider whether the airway is “safe” or not. If it is compromised, the local anaphylaxis protocol should be followed and mechanical intervention may be needed, either by intubation or cricothyrotomy/tracheotomy [4]
The mechanism underlying ACEI-induced angioedema (excess bradykinin) is similar to that underlying HAE. For that reason, agents shown to be effective in HAE are currently being investigated in clinical studies as treatments for acute ACEI-induced angioedema.
Several small case studies have reported on the use of icatibant (bradykinin receptor antagonist) for the treatment of ACEI-induced angioedema [5, 6].
Unfortunately these agents are very costly and not licenced for treatment of this condition. Anecdotally in my clinical practice I noticed some improvement in symptoms with conventional treatment like anti histamines and steroids.
ACE inhibitors should be immediately stopped. Angiotensin receptor blockers (ARB) should be avoided as well (in these patients) as they are also known to induce angioedema.
When it is safe to discharge patients?
Patients with ACE inhibitor angioedema with the swelling confined to lips should be observed for 4 to 6 hours and then can be discharged home (with safety advice) if symptoms are resolving or at least not worsening. All other patients should be admitted till the resolution of symptoms (usually 24 to 72 hours).[7]
References:
1.Emerging concepts in the diagnosis and treatment of patients with undifferentiated angioedema.
Bernstein JA, Moellman J
Int J Emerg Med. 2012 Nov 6; 5(1):39.
2.Pathways for bradykinin formation and inflammatory disease.
Kaplan AP, Joseph K, Silverberg M
J Allergy Clin Immunol. 2002 Feb; 109(2):195-209.
3.Temiño VM, Peebles RS: The spectrum and treatment of angioedema. Am J Med 2008, 121: 282–286. 10.1016/j.amjmed.2007.09.024
4.Acute angioedema: recognition and management in the emergency department.
Jaiganesh T, Wiese M, Hollingsworth J, Hughan C, Kamara M, Wood P, Bethune C
Eur J Emerg Med. 2013 Feb; 20(1):10-7.
5.Angioedema induced by angiotensin-converting enzyme inhibitors: two cases of successful treatment with a novel B2 bradykinin antagonist
Perez DV, Infante S, Marco G, Zubeldia JM, Marañon G:
[AAAAI Abstract]. J Allergy Clin Immunol 2011,27(2):AB105.
6.Therapeutic efficacy of icatibant in angioedema induced by angiotensin-converting enzyme inhibitors: a case series.
Bas M, Greve J, Stelter K:
Ann Emerg Med 2010,56(3):278–282. 10.1016/j.annemergmed.2010.03.032
7.Emergency department evaluation of patients with angiotensin converting enzyme inhibitor associated angioedema.
Mudd PA, Hooker EA, Stolz U, Hart KW, Bernstein JA, Moellman JJ.
Am J Emerg Med. 2020 Dec;38(12):2596-2601. doi: 10.1016/j.ajem.2019.12.058. Epub 2020 Jan 7. PMID: 31932133.