82 years old man was brought to A&E department by ambulance with history for confusion and drowsiness for past few days. He lived in sheltered accommodation and the carer had called ambulance. No further history was available. He had past medical history of cirrhosis of liver, hypertension and IHD.
On examination he was drowsy and confused (GCS-13/15, E3 V4 M6).
Examination findings are as follows:
Temp. 37.8 C
PR- 90/ min
BP- 106/ 60 mm Hg
Heart and lung examination was normal.
Abdominal exam- generalised distension with shifting dullness suggestive of ascites.
CNS- GCS-13/15, pupils- PEARLA, no focal neurological deficits.
Blood glucose: 7.8 mmol/L
Does ammonia level help in the diagnosis and management of suspected hepatic encephalopathy?
My learning:
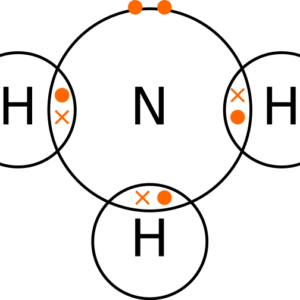
The gastrointestinal tract is the primary source of ammonia, which enters the circulation via the portal vein.
Ammonia is produced by enterocytes from catabolism of ingested proteins. The intact liver clears almost all of the portal vein ammonia, converting it into urea or glutamine.
The increase in blood ammonia levels in advanced liver disease is a consequence of impaired liver function and of shunting of blood around the liver.
The diagnosis and staging of hepatic encephalopathy is based on clinical examination. Investigations are necessary to exclude other causes of mental status alteration.
Utility of ammonia levels is limited. High ammonia levels do not have diagnostic, staging, or prognostic value for patients with hepatic encephalopathy [1,2].
Monitoring ammonia trends may be helpful in monitoring therapy, but it is not required to make a diagnosis.
The severity of hepatic encephalopathy is graded based on the clinical manifestations.
- Grade I: Changes in behaviour, mild confusion, slurred speech, disordered sleep
- Grade II: Lethargy, moderate confusion
- Grade III: Marked confusion (stupor), incoherent speech, sleeping but arousable
- Grade IV: Coma, unresponsive to pain
Note:
Above information is based on the “Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver”.
I have also also consulted Uptodate and BMJ best practice websites (references below)
Thee is no specific NICE guideline for this situation.
NCIC trust guideline does not advice checking ammonia level as part of evaluation of decompensated liver disease.
Bottom line:
I do not routinely check serum ammonia levels in patients with suspected hepatic encephalopathy.
References:
- https://bestpractice.bmj.com/topics/en-gb/294/diagnosis-approach
- https://www.uptodate.com/contents/hepatic-encephalopathy-in-adults-clinical-manifestations-and-diagnosis?source=history_widget#H152815085
- Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, Weissenborn K, Wong P. Hepatic encephalopathy in chronic liver disease: 2014Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014 Aug;60(2):715-35. doi: 10.1002/hep.27210. Epub 2014 Jul 8. PMID: 25042402.
- Cordoba J, Ventura-Cots M, Simón-Talero M, Amorós À, Pavesi M, Vilstrup H, Angeli P, Domenicali M, Ginés P, Bernardi M, Arroyo V; CANONIC Study Investigators of EASL-CLIF Consortium.Characteristics, risk factors, and mortality of cirrhotic patients hospitalized for hepatic encephalopathy with and without acute-on-chronic liver failure (ACLF). J Hepatol. 2014 Feb;60(2):275-81. doi: 10.1016/j.jhep.2013.10.004. Epub 2013 Oct 12. PMID: 24128414.